Case Study: How Camber’s Technology-Enabled Service Helped a Multi-Disciplinary Clinic Scale by 60% in Two Years
"We felt a strong philosophical alignment with Camber from the start. They understood our approach to growth and problem-solving, and they shared our belief that success comes from continuously iterating and improving together. It wasn’t just about fixing immediate issues; it was about building a long-term solution."
— Rick McKellar, CFO of Gracent
Growing Potential
Gracent, a leading provider of multidisciplinary pediatric therapies throughout Illinois (Chicago) and Texas (Dallas-Fort Worth) areas, was formed through the merger of North Shore Pediatric Therapies and Pine Cone Therapies, with a mission to enhance patient-centered care. They specialize in applied behavioral analysis (ABA), neuropsychological testing, speech therapy, occupational therapy, mental health services, and physical therapy. Operating under the philosophy of “Together, We Grow Potential,” the company views growth not just as financial success but as an expansion of opportunities for children, staff, and the organization as a whole.
The Need for Change
Between 2023 and 2024, Gracent experienced rapid growth, 30% in 2023 and 25% in 2024, resulting in a 60% expansion over two years. However, as Gracent scaled, its revenue cycle management (RCM) infrastructure struggled to keep pace.
Their reliance on a conventional outsourced billing vendor led to mounting inefficiencies, particularly as labor market fluctuations impacted vendor staffing. Leadership needed a partner capable of managing billing operations at scale while also providing visibility into financial performance.
After evaluating multiple solutions, including an in-house approach and other service-driven vendors, Gracent selected us for our ability to blend automation with hands-on strategic support. Unlike traditional billing providers, we operate as a technology-enabled service partner, allowing Gracent to achieve financial stability while positioning the organization for continued expansion.
Key Challenges & Transformations
Challenge #1: Scaling Without Labor Market Vulnerabilities
Gracent’s previous billing partner struggled with workforce disruptions, leading to inconsistent cash flow and operational bottlenecks. Without a strong technology backbone, their revenue cycle was heavily dependent on manual processes, making it difficult to scale efficiently.
We implemented a technology-driven RCM model that automated key billing workflows, reducing reliance on manual labor while improving efficiency for over 2,500 patients. Tasks such as claims submission, denials management, payment posting, and patient invoicing were streamlined, allowing Gracent’s internal RCM team to scale without significantly increasing headcount.
In addition to automation, we enhanced patient collections by enabling automated weekly invoicing and auto-charging. This eliminated administrative burdens while ensuring a seamless, predictable payment experience for both parents and staff.
As Gracent’s patient volume grew by 60%, they needed a scalable strategy that didn’t rely solely on hiring. We worked closely with their team to bring key billing functions back in-house, such as credentialing, while also implementing operational frameworks that improved efficiency in areas requiring human oversight. These changes not only reduced outsourcing costs but also freed billing staff to focus on higher-value initiatives, like payer negotiations and patient financial support.
By integrating intelligent automation, we stabilized revenue operations and minimized the risk of collection delays due to workforce shortages. Additionally, our payer-specific validation rules and structured workflows increased Gracent’s first-pass pay rate by 10 percentage points within 60 days, reducing costly resubmissions and accelerating cash flow.
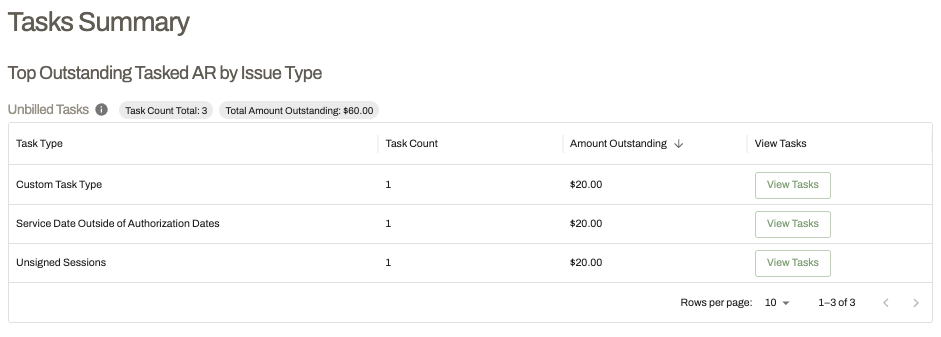
Caption: Camber’s task module simplifies and siloes tasks that require human touch into ‘Task Type’
Challenge #2: Lack of Transparency and Proactive Revenue Cycle Management
Gracent’s leadership lacked real-time insight into its revenue cycle. Without a structured reporting system, executives were left making decisions based on incomplete or outdated data.
We deployed a reporting module and dynamic task management system that provided real-time visibility into financial performance. With proactive tracking tools, leadership could identify revenue cycle bottlenecks before they impacted cash flow. As their Director of RCM summarized:
"They hear our feedback and do something with it. We can say, 'This process isn’t working,' or 'We need to revamp this entirely,' and they take that and implement it."
The feedback loop was immediate. Leadership no longer had to rely on fragmented reports or reactive responses from a third-party vendor. Instead, they had on-demand access to performance metrics, denial trends, and ERA monitoring—enabling them to make data-driven decisions.
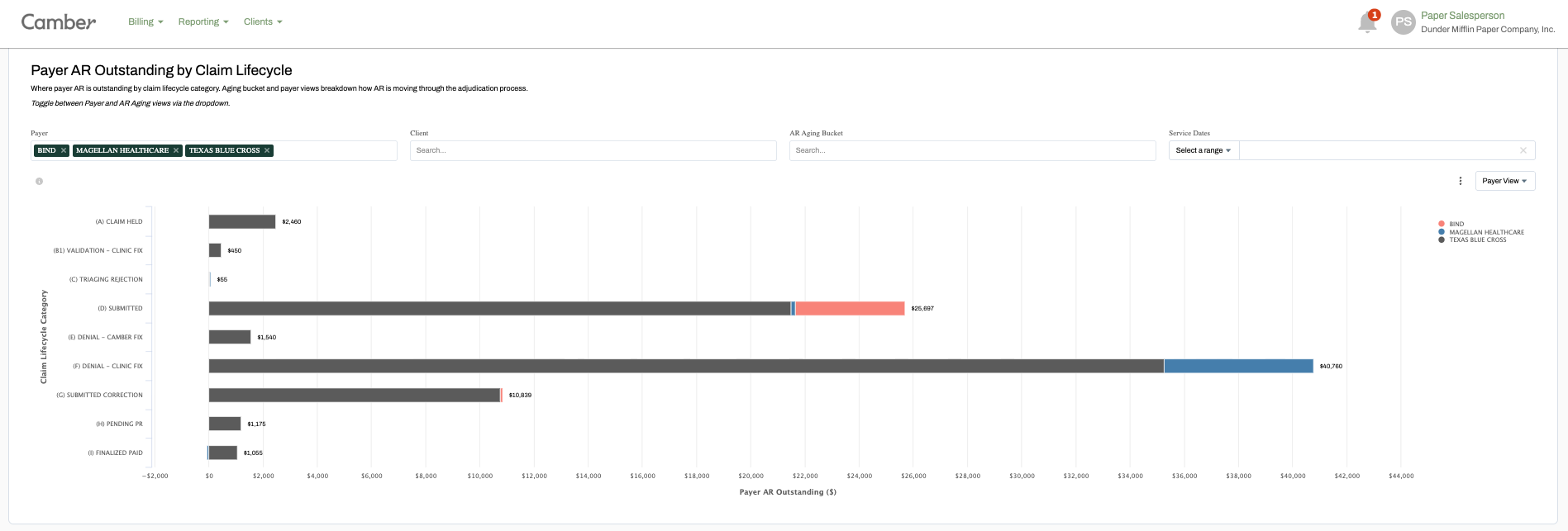
Caption: Camber’s dashboard on AR outstanding by payers and by step of claim lifecycle
This level of transparency not only improved operational efficiency but also strengthened financial planning, allowing Gracent to allocate resources more effectively as they scaled.
What’s Next?
Gracent’s decision to partner with us was not just about fixing short-term inefficiencies, it was about building a sustainable, scalable revenue cycle strategy to support long-term growth. With a modernized RCM infrastructure in place, the company is now focused on expanding its multidisciplinary services while maintaining a high standard of patient-centered care.
Our partnership gives Gracent real-time data visibility, automated revenue cycle processes, and a proactive compliance framework, taking their mission, 'Together, we grow potential,' to the next level.
Seeing Similar Inefficiencies?
If you’re looking to scale and expand quality care while improving your revenue cycle, get in touch with us today. Schedule a call to hear how a partnership with us can help you transform your billing operations.